Scientists have taken skin cells from a woman suffering from type 1 diabetes, reprogrammed them into embryonic stem cells, and then converted those cells into insulin-producing cells in mice, according to a new study.
The announcement, which comes soon after another stem cell success involving therapeutic cloning, was published Monday in the journal Nature.
“This advance brings us a significant step closer to the development of cell replacement therapies,” said senior study author Dieter Egli, a researcher at the New York Stem Cell Foundation.
Embryonic stem cells, or pluripotent cells, are cells that can reproduce endlessly and transform themselves into any type of human tissue. Researchers hope that the cells will one day be used to create transplant tissues that will not be rejected by the patient’s body, because they carry their own DNA.
Egli and his colleagues used a cloning technique known as somatic cell nuclear transfer, or SCNT — a process similar to the one used to clone “Dolly” the sheep in 1996.
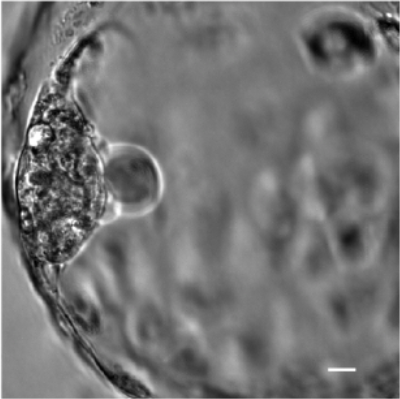
The process involves removing the nucleus from a human egg cell, replacing it with the nucleus from a foreign “donor” cell, and then allowing the egg to divide and develop for a period of days. The developing embryo will contain a mass of pluripotent cells, which are removed and used to create a line of reproducing cells.
If the cloned embryo were implanted in the womb of a surrogate mother — an act scientists consider unethical for a number of reasons — it could possibly develop into a baby.
Up until now, the stem cell field has relied on a very different method of pluripotent cell production called induced pluripotency. The process is viewed as being much easier than SCNT, because it does not involve the controversial use of human egg cells, which are also difficult to obtain.
At a news conference, Egli told reporters that the SCNT process was becoming increasingly refined and should be viewed as a reliable source of pluripotent cells.
“For me this is the way to go,” Egli said. “This is about reprogramming a patient’s own cells, with their own genotype, with their own DNA that are immunologically matched to them and no one else, essentially. I think this is going to become a reality.”
Egli and his colleagues used donor skin cells from a 32-year-old woman who has had type 1 diabetes since she was 10 years old.
In type 1 diabetes, a patient’s pancreas stops producing insulin. In healthy individuals, that hormone allows glucose to enter cells and be used to produce energy.
The pancreatic cells that produce insulin are called beta cells, and researchers set out to demonstrate that their pluripotent cells could become beta cells.
After harvesting pluripotent cells from the cloned embryos, they were then transplanted into mice. The mice suffered from weak immune systems, so that their bodies would not reject the human stem cells.
Study authors said the human stem cells gave rise to both nerve cells and beta cells within the mice.
While the study is encouraging, it remains unclear when similar stem cells can be implanted into humans.
Egli said the process has yet to be perfected in mice, and that he and his colleagues were now working on this. The problem, he said, was that when the beta cells were created, other cells also appeared.
“One of the main obstacles that still hold back this field is that we cannot make one and only that one cell type, without any other contaminating cells,” Egli said. “So learning how to better control that, and perhaps eliminate that, is going to be key.”
Like other researchers, Egli and his colleagues found that eggs from younger women — age 21 to 26 — were most likely to produce usable embryos.
They also found that they had more luck cloning embryos when they delayed cell division after introducing the donor nucleus.
While other researchers have used caffeine to delay cell division, a trick they have dubbed “the Starbucks effect,” Egli said he and his colleagues had better luck using histone deacetylase inhibitors, which essentially block the activity of certain enzymes.
“It is entirely possible that the caffeine has a beneficial effect, but its not the magic factor that makes or breaks this method,” Egli said.
(via LA Times)